Hannah Yoon | The Washington Post | Getty Images
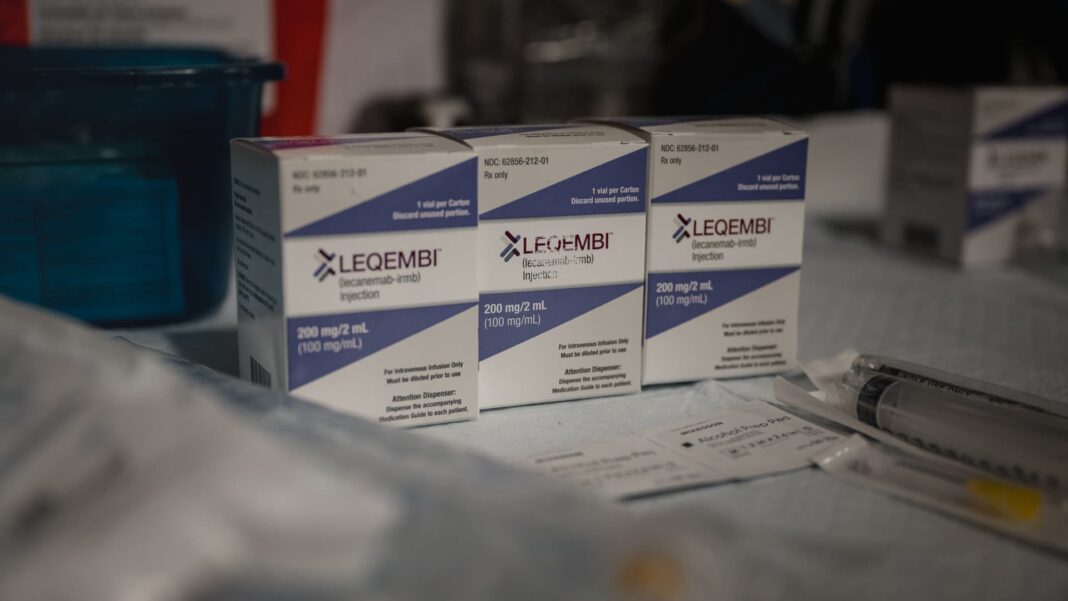
Leqembi, an Alzheimer’s drug from Biogen and Eisai, isn’t a cure for the mind-damaging disease.
But the treatment promises to give patients such as Missie Meeks more time to live their daily lives normally and independently of others.
Meeks, an English professor based in Ellisville, Mississippi, was diagnosed with an early stage of Alzheimer’s last summer ahead of her 50th birthday. That eventually made her a good fit for Leqembi, which won regulatory approval in the U.S. in July 2023.
Meeks received her first infusion of Leqembi in September 2023 after overcoming a few logistical hurdles, such as securing an appointment with a neurologist and getting insurance to cover the costly treatment, which it initially denied because of her age. Since then, she has been taking infusions of the drug every two weeks.
Meeks is no longer teaching, but she said Leqembi is “extending my time of a normal life.”
“I still have fumbles. I’m not perfect by any means. But I can function every day pretty much normally. I can drive, I can go to the doctor, I can go out to eat,” Meeks told CNBC. “It’s extending my time of a normal life.”
Leqembi is considered a breakthrough for a progressive disease that has proven notoriously hard to treat. Leqembi is a monoclonal antibody that moderately slows the decline in memory and thinking in patients in the earliest stages of Alzheimer’s. Only a narrow swath of the nearly 7 million U.S. patients with the disease are in those early phases.
Still, the drug carries risks of brain swelling and bleeding. Some neurologists and other experts also say patients taking the drug haven’t had it long enough to see a substantial clinical benefit, which was observed at 18 months in Biogen and Eisai’s late-stage trial.
Meeks’ experience also points to the new and complicated system associated with taking Leqembi, which has hampered the drug’s rollout. There are bottlenecks related to reimbursement uncertainties, diagnostic test requirements, the need for regular brain scans and difficulties finding neurologists. Some hospitals and clinics simply aren’t equipped to accommodate the new flow of patients who could take the drug.
Some doctors are also reluctant to prescribe Leqembi, citing their concerns about its risks and skepticism around how much it meaningfully benefits patients.
Some experts say those issues partly reflect the steep learning curve that comes with a new drug such as Leqembi, which has ushered in a new era for the Alzheimer’s treatment space.
“Every time there’s new technology or medication, it puts a little stress on the system, because change is hard,” said Dr. Julio Rojas, a professor and behavioral neurologist who is involved with administering Leqembi at the University of California, San Francisco Health. “We’re still figuring out how to use the drug, how to monitor it, when to stop it, how to decide if it’s working or not.”
Nonetheless, some patients and their caregivers say the risk and grueling process is worth it.
“I know Leqembi does not cure Alzheimer’s. The focus is to stop the progression,” said Meeks’ mother, Patricia Waldrup. “She has two children, and she’ll have more time to enjoy their lives and her husband’s life. … We have praises for that.”
Meanwhile, the number of patients taking Leqembi appears to be increasing.
The treatment raked in nearly $60 million in sales for the first half of the year, up from the $10 million the drug brought in during its first year on the market in 2023, according to Biogen’s first and second quarter earnings reports. In Biogen’s most recent update, in May, it said roughly 5,000 people were taking the drug at the time.
A long road to diagnosis
Leqembi’s rollout has been gradual in part due to the arduous process involved in diagnosing a patient with mild cognitive impairment or mild dementia, the earliest two stages of Alzheimer’s.
Alzheimer’s is the most common form of dementia, a general term for loss of memory, language and other thinking abilities.
Brian B. Bettencourt | Toronto Star | Getty Images
Tracey Collins, a global public relations officer based in Portland, Maine, said it took her roughly 2½ years to receive a diagnosis for early Alzheimer’s after she started experiencing symptoms of cognitive decline, such as memory loss.
Collins, 54, said that was in part due to her being younger than the typical Alzheimer’s patient and her physician attributing symptoms to other factors, such as trauma from recent family-related issues and attention-deficit/hyperactivity disorder.
Collins was also recovering from a benign meningioma — a non-cancerous tumor that forms in tissue covering the brain and spinal cord — which can also cause cognitive dysfunction. But Collins’ physician eventually referred her to a neurologist in Boston who performed a spinal fluid test to diagnose her with early Alzheimer’s in 2022.
Simply finding a neurologist can be a difficult task, since there are not enough of them practicing in the U.S., Alex Scott, Eisai’s chief administrative officer, told CNBC.
“Once you are told to go see a neurologist, guess what? That puts you in the position of waiting anywhere between four and eight months or so to get to see one,” Scott said.
That was the case for Meeks, who said she waited a few months to get her first appointment with her neurologist in South Mississippi.
A 2020 study of Medicare enrollees found that only 24% of patients with a neurologic condition were seen by a neurologist, with notable regional differences. For those with dementia, 38% of people in more rural areas saw a neurologist, compared with 47% in urban areas.
Eligibility and insurance bottlenecks
Even after a diagnosis, patients and neurologists must jump through several hoops to determine eligibility for Leqembi, experts say.
The drug works in part by clearing toxic plaques in the brain called amyloid, a hallmark of Alzheimer’s, according to its manufacturers. That means patients must undergo a PET scan or a spinal fluid test to determine if amyloid has accumulated in their brains.
Patients typically prefer PET scans, which are painless, for detecting amyloid, according to Scott. But, he said, Medicare only decided to broaden coverage of those scans for Alzheimer’s in October, which contributed to Leqembi’s sluggish initial launch.
Neurologists also perform an MRI scan to ensure that patients don’t have other brain diseases that may be causing cognitive issues, Dr. Ronald Petersen, the director of the Mayo Clinic Alzheimer’s Disease Research Center, told CNBC. Neurologists use the MRI to evaluate whether patients have microbleeds in their brains, which could make them ineligible for Leqembi because it puts them at a higher risk of its serious side effects, according to experts.
Jay Reinstein, a patient with Alzheimer’s, sits on a bed after receiving a PET scan at MedStar Georgetown University Hospital in Washington, D.C., June 20, 2023.
Michael Robinson Chávez | The Washington Post | Getty Images
Some hospitals and clinics also require genetic testing for two copies of the so-called APOE4 gene variant, which is also associated with an increased risk of brain swelling and bleeding, according to experts and Eisai. Those side effects are also known as amyloid-related imaging abnormalities, or ARIA.
Once those tests are complete, a panel of 20 to 30 neurologists, radiologists, psychiatrists and other experts vote on whether they think a patient qualifies for treatment with Leqembi, Petersen said, referring to the process at the Mayo Clinic’s Alzheimer’s center.
He said roughly 60% of people evaluated by the Mayo Clinic’s panel end up being eligible for the treatment and that most of those patients agree to take it. The Mayo Clinic’s center, which began screening patients for Leqembi in October, has 50 to 60 patients currently taking the drug, according to Petersen.
Petersen said the center evaluates three to five new patient referrals at the beginning of each week and his team determines whether they are eligible for Leqembi by Thursday.
Still, Petersen said it can take months for a patient at the Mayo Clinic to receive Leqembi due to other hurdles, such as insurance issues.
While Medicare covers Leqembi, some patients who aren’t old enough to enroll in the federal program may struggle to get coverage. Some commercial health plans simply don’t cover the drug, experts say, which has a $26,500 annual price tag before insurance.
Collins, the patient from Portland, said her insurance denied her request for Leqembi coverage three times, delaying her ability to start taking the drug. She was referred to a neurologist in April 2023 and received her first infusion in January.
It can take other patients even longer, particularly if they are going to health centers that aren’t fully equipped to perform MRI scans or other requirements.
Michael Irizarry, Eisai’s senior vice president of clinical research, acknowledged the lengthy process that patients have to undergo to receive Leqembi. But he noted that “all those steps are completely new, essentially since the approval of [Leqembi], and really is a transformation in the care of these patients.”
Infusion clinics can be hard to find
Once a patient gets coverage for Leqembi, they can start biweekly intravenous infusions of the drug. But some neurologists don’t have infusion clinics in their office, so they have to send patients to another health center that does.
In some cases, the nearest infusion clinic may be dozens of miles away, which can be a huge obstacle for patients and caregivers who don’t have reliable access to transportation or time to drive to another location.
An analysis published in April by Being Patient, an online news source dedicated to Alzheimer’s disease, estimated that there are more than 850 infusion sites in the U.S. offering Leqembi. But the analysis found that 11 states had five or fewer infusion clinics administering the drug.
A spokesperson for Eisai did not provide a specific number of Leqembi infusion clinics in the U.S. but noted that the company has a tool that helps patients locate sites in the U.S. near them.
But Eisai and Biogen said they are working on more convenient forms of Leqembi that could reduce the burden on patients and their caregivers and potentially expand uptake.
The companies are hoping to win regulatory approval for a so-called “maintenance dose” of Leqembi, which would stretch infusion intervals to once per month after an initial period of receiving biweekly infusions.
Eisai’s Scott added that the company is hoping to win regulatory approval for a version of Leqembi that is injected weekly under the skin at home or in a medical facility. The approval would allow patients to eventually switch to that subcutaneous form of the drug as a maintenance dose of Leqembi.
Collins drives 20 minutes to her primary care doctor in South Portland to receive Leqembi infusions, which she said feels like “a spa day” despite having an IV in her arm for almost an hour.
“They give me coffee, snacks, and I sit and read on reclining chairs. I kind of make it a fun event,” she said. “My kids have sometimes come to hang out with me. It’s not really in a hospital setting so it doesn’t feel scary.”
Meeks said her infusions feel like “therapy sessions” because she gets to talk to other patients and their caregivers at her clinic about their experiences with the disease.
“It’s just comforting to hear other people’s stories as you sit in there,” Meeks said, adding that the roughly 40-minute infusion is “done before you know it.”
Patients may experience infusion-related reactions during their first two sessions, such as flu-like symptoms, according to Irizarry.
Neurologists also conduct regular MRI scans on patients to monitor for ARIA, or brain swelling and bleeding, side effects, according to Eisai.
Side effects
Leqembi has so far been well-tolerated by patients, according to Rojas. But he said the risk of ARIA is “always in the back of our head at all times.”
UCSF’s clinic will have patients skip infusions of Leqembi until ARIA goes away, or use steroids to decrease brain inflammation.
The Mayo Clinic’s Alzheimer’s center similarly stops dosing patients if ARIA appears on an MRI, according to Petersen. The center has seen a few cases of those side effects, but “nothing too dramatic, nothing fatal,” he said.
“Our experience thus far has generally been positive,” Petersen said.
Meeks’ neurologist, Dr. Wendell Helveston, said a follow-up MRI picked up one small area of bleeding in her brain that didn’t cause any symptoms.
Helveston, who practices at the Hattiesburg Clinic in Mississippi, said Meeks’ bleeding was “well below the level where we would need to stop dosing” Leqembi.
He also said Meeks’ rate of cognitive decline has stabilized after several months of treatment, which is “exactly what we would like to see” from patients taking the drug.
The promise of Leqembi
But even as uptake of the drug ramps up, Petersen said it may still be too early to say how much patients are benefiting from the drug.
Leqembi reduced cognitive decline by 27% after 18 months in Biogen and Eisai’s pivotal late-stage trial – data that supported the treatment’s approval in 2023. Eisai in July also released new data showing that the progression of the disease in patients on Leqembi continued to slow after three years, suggesting the need for them to take the treatment long-term.
Mr. Bobby Pugh, 91, cares for his wife Bessie Pugh, 90, an Alzheimer’s patient at the Ave Maria Home, an assisted living center for seniors, in Bartlett, Tennessee, U.S., September 13, 2023.
Karen Pulfer Focht | Reuters
But it’s only been roughly 14 months since Leqembi was approved, and some patients have been taking the drug for an even shorter period of time.
“We’re not out that far yet to really see if people are remaining relatively stable,” Petersen said. “Subjectively, it looks like it, but that’s really a soft criterion at this time. So we’re just going to continue on and evaluate our experience at the end of the 18 months.”
Meanwhile, patients such as Collins are pinning their hopes on Leqembi to give them extra time to live independently and perform their usual daily activities.
“Having something that can keep me living in my environment, doing my job and being able to take care of teenagers — it’s what gets me through the next week,” she said.